
TIMELY FILING APPEAL LETTER CODE
To file an appeal, you must submit the final deadline appeal request electronically via Direct Data Entry. In order for your appeal to be approved, you must demonstrate that the claim was denied or underpaid as a result of a MassHealth error, and could not otherwise be timely resubmitted. You must file the appeal within 30 days of the date that appears on the remittance advice on which your claim first denied with error code 853 or 855. To be eligible for appeal, your claim must have been denied for error code 853 or 855 (Final Deadline Exceeded). When a claim or adjustment request meets one of the exceptions to the submission deadline, the provider is required to mail ForwardHealth a Timely Filing. A claim with this error code cannot be appealed.Īppeal procedures for error codes 853 or 855 ('Final Deadline Exceeded')

If the date of service is more than 36 months when it is received by MassHealth, the claim will be denied for error 856 or 857 (Date of Service Exceeds 36 Months) on an RA. you may appeal the claim adjudication decision if timely filing rights. The form provided above is just the first page in the appeal form provided by Medical Mutual. See the following section for the appeal procedures for these error codes CareSource will render a claim dispute decision letter within 30 calendar days of. Lack of timely filing appeals and using affidavits for establish timely filing. If you exceed this deadline, your claim will be denied for error code 853 or 855 (Final Deadline Exceeded) on an RA. You have 18 months from the service date to resolve your claim, as long as the claim was received by MassHealth within 90 days of the EOB date. If you exceed this deadline, your claim will be denied for error code 853 or 855 (Final Deadline Exceeded) on an RA. See the following section for the appeal procedures for these error codesįinal submission deadline if you had to bill another insurance carrier before billing MassHealth. You have 12 months from the date of service to resolve your claim, if you originally submitted the claim within 90 days from the date of service. Appeals Appeals may be initiated in writing or by telephone, upon receipt of a denial letter and instructions from BCBSMT. These requests are subject to the non-formulary exception process described later in this section. This grievance/appeal process does not apply when a Member is requesting coverage of a Drug or item not listed on Our formulary. Please submit the appeal online via Availity Essentials or send the appeal to the following address: Humana Grievances and Appeals P.O. All expedited grievances/appeals will be resolved within 72 hours of the time We receive your request. If you had to bill another insurance carrier before billing MassHealth, you have 90 days from the date of the explanation of benefits (EOB) of the primary insurer to submit your claim.įinal submission deadline. If filing on your own behalf, you need to submit your written request within the time frame established by applicable state law. Initial claims must be received by MassHealth within 90 days of the service date. Usual turnaround time for Medicare/MassHealth crossover claims forwarded to MassHealth by the Massachusetts Medicare fiscal agent to be processed. This letter is called a notice of Adverse Benefit Determination letter (formally known as Notice of Proposed Action letter or a denial). Hoping to hear from you soon in this context.Average time for both electronic (EDI) and paper claims to process on a remittance advice (RA).
TIMELY FILING APPEAL LETTER FREE
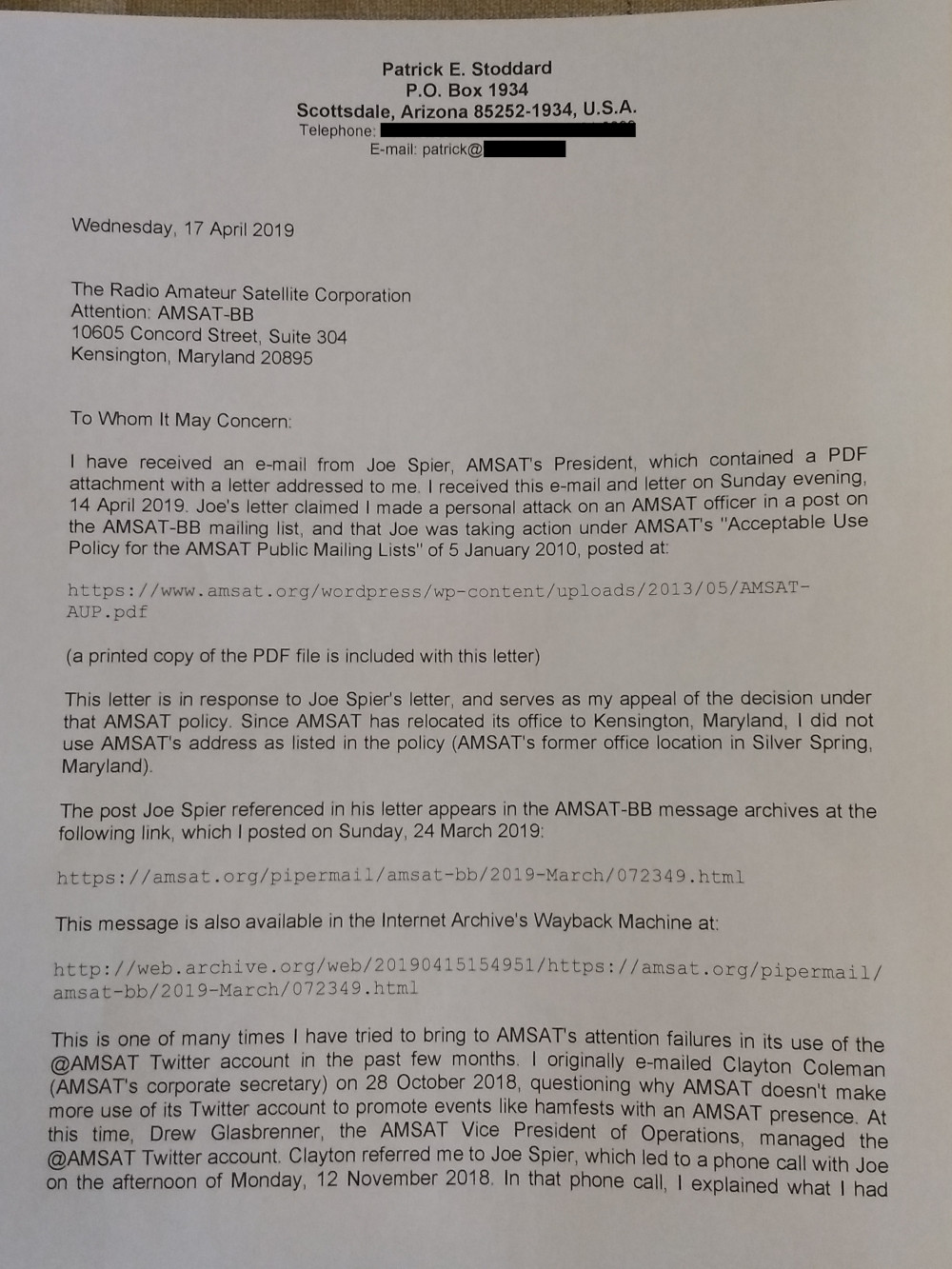
If you have any clarifications on this, please feel free to call us at (phone number) Also we would be left out with no other option except to go ahead and bill the patients for these if we do not hear back from you. In this context, we request you to kindly have these claims re-processed and expedite reimbursements on these claims. We are having all these accounts sitting in our books as outstanding for no fault of ours. But as per our records the claims had been submitted within the timely filing limit deadline and we have attached all the details herewith. We had already submitted claims to you for the patients (Patient names) but the claims has been denies for lapse in timely filing limit. Sub.: Appeal of Medical claims pertaining to Dates of Service ……………………


 0 kommentar(er)
0 kommentar(er)
